Robotics-assisted knee surgery with Smith+Nephew implants can deliver the ultimate knee replacement experience – a quicker, smoother recovery*1,2†using a naturally shaped knee made from materials designed to last.
Knee replacement has changed-for the better
The earliest knee replacement procedures were performed in 1968 and relied on manual guides and procedures to remove damaged bone and place the implant within the joint.
Over time, more advanced implant techniques were introduced that used long metal alignment rods inserted into the center of the thigh bone (femur). These rods, which help determine the correct anatomic alignment between the knee and hip, provide an attachment point for positioning the surgical cutting guides. Once the bone cuts are made, the surgeon must remove these rods before the new implant can be positioned. More recently, pre-surgery improvements like computerized tomography (CT) scans and magnetic resonance images (MRIs) are now used to help create computer-generated surgical plans for each patient.
However, even with these advances, drawbacks still remain. For example, the use of alignment rods may lead to a risk of surgical complications such as fat embolisms3, CT scans can result in potentially harmful radiation exposure, and pre-surgical MRIs may increase overall costs or add time from consultation to procedure.
The ultimate knee replacement experience
Enter robotics-assisted surgery: combining the advantages of traditional methods with innovations while minimizing the drawbacks to patients. This advanced technology is designed to help me plan and perform your knee replacement surgery with a greater degree of accuracy than is possible with traditional methods,4-8 and without the need for metal rods, CT scans or pre-surgical MRIs. Smith+Nephew, the only company offering handheld robotics assisted technology for partial and total knee replacements, believes this enhanced level of accuracy can give you a better long-term outcome.4-6,9
A unique plan
Your knee replacement surgery is as unique as you are because it’s the only one that combines your knee’s anatomy with the specific implant I have chosen for you. As a result, your surgery requires an individualized surgical plan to help ensure your implant is positioned and aligned correctly for your anatomy. With robotics-assisted surgery, I use the CORI◊ Surgical System to create a customized 3D digital model of your knee. This three-dimensional view helps me finalize and verify the right size implant for you and create a detailed surgical plan for how your replacement will be placed in order to optimize movement and function. As an added benefit, the 3D digital model eliminates the need to get a CT scan of your knee before your surgery, which reduces your exposure to harmful radiation.
A natural fit
 Of course, robotics-assisted surgery is about more than a detailed 3D view of your knee. The CORI Surgical System also helps me perform the procedure as I planned it, giving you the combined benefits of the accuracy of robotics assistance and the skill and training I have developed.5,6,10,11
Of course, robotics-assisted surgery is about more than a detailed 3D view of your knee. The CORI Surgical System also helps me perform the procedure as I planned it, giving you the combined benefits of the accuracy of robotics assistance and the skill and training I have developed.5,6,10,11
When it comes to knee replacement surgery, accuracy is important because if an implant is positioned incorrectly, it may not function as well as it should nor last as long as possible. In addition to its added accuracy, when robotics-assisted surgical procedures are combined with the wide variety of Smith+Nephew implants available, I am able to choose the implant which best meets your needs, including options that allow you to keep more of your natural bone and ligaments, including the ACL.12 That means your body can maintain more of its natural rhythm and step.12,13 You may also regain function faster and get discharged from the hospital sooner as compared to conventional technique surgeries.* 13‡
A wide selection
 Knee replacement shouldn’t be a one-size-fits-all. With the CORI robotics-assisted surgical system, I am able to choose your implant from the widest selection available.14 Moving beyond the variety of options available, only Smith+Nephew knee implants can be made with a highly durable material called OXINIUM◊ Oxidized Zirconium. This unique, innovative material has been lab tested to last significantly longer than conventional knee implant materials.14,15
Knee replacement shouldn’t be a one-size-fits-all. With the CORI robotics-assisted surgical system, I am able to choose your implant from the widest selection available.14 Moving beyond the variety of options available, only Smith+Nephew knee implants can be made with a highly durable material called OXINIUM◊ Oxidized Zirconium. This unique, innovative material has been lab tested to last significantly longer than conventional knee implant materials.14,15
Why does my knee hurt?
One of the most common reasons for knee pain is osteoarthritis, also known as “wear and tear” arthritis. This disease often requires treatment using either full or partial knee replacement surgery. Generally speaking, as osteoarthritis progresses it causes the smooth cushion between bones (cartilage) to break down. This loss of cartilage can cause your joints to become swollen, hard to move and painful.17 While there’s no cure for osteoarthritis, there are lots of treatment options, including both surgical and nonsurgical options we should discuss. These include:
- Lifestyle changes that can include weight loss and reducing activities that are stressful on your knee
- Physician-prescribed low-impact exercises and physical therapy
- Medications to decrease swelling and provide temporary pain relief
- Surgical options, such as arthroscopic surgery, and partial and total knee replacement
Total knee replacement with the CORI Surgical System
Most often, this procedure is an option for advanced knee pain and damage. With this type of knee implant I replace the entire knee joint. It’s one of the most common procedures performed in all of medicine.
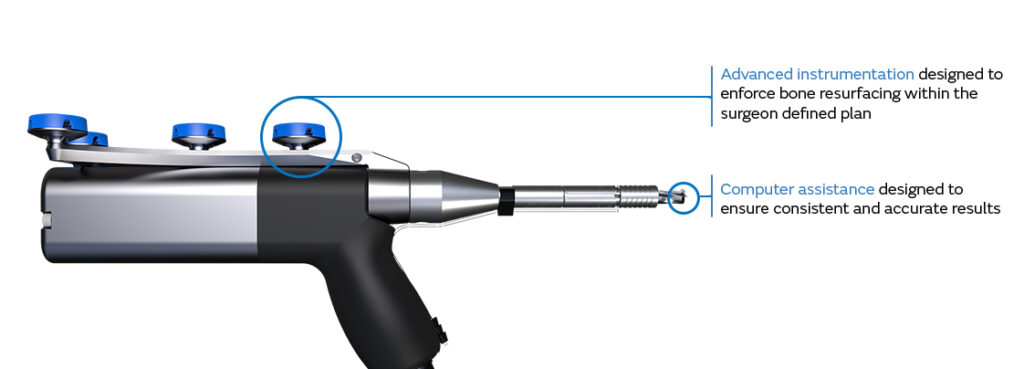
Since no two knee joints are the same, aligning your new knee implant requires me to match its position with your knee’s existing range of motion. The CORI System uses a robotics-assisted, handheld device – placing an additional layer of planning and accuracy directly into my hands.
Traditional surgical techniques still use rods and older methodology.
CORI Surgical System
When the skills and training I have developed combine with the latest in robotics-assisted and knee implant technology, you can rest easy knowing you’re getting the ultimate knee replacement experience.
The CORI Surgical System uses handheld robotics-assisted technology that helps me plan and perform your unique procedure. This robotics-assisted approach is efficient and more accurate than traditional knee surgery.5,6,8
At the beginning of your surgery, I use the CORI system to create a customized 3D digital model of your knee. This three-dimensional view helps me finalize and verify the selection of your knee implant and create a plan for your surgery without the need for either a CT scan or MRI.
During the procedure, the CORI system works in conjunction with my surgical training to achieve accurate positioning of the knee implant based on your unique anatomy.7,10,11,18,20,21The system sends precise information about your knee to the robotics-assisted handpiece more than 300 times per second, allowing me to remove damaged surfaces, balance your joint and position the implant with accuracy. 7,10,11,18,20,21
The result is a naturally shaped knee, made from materials designed to last longer, that is positioned with an added level of accuracy to allow for a quicker, smoother recovery*1,2†
Important safety notes
Not all patients are candidates for the Smith+Nephew knee products. Knee replacement surgery is intended to relieve knee pain and improve knee functions. Implants may not produce the same feel or function as your original knee, and individual results will vary. Potential risks include loosening, wear and infection that may result in the need for additional surgery. There are risks associated with any surgical procedure including CORI-enabled Knee Replacement. The CORI Surgical System is not for everyone. Discuss your condition and implant options with your surgeon to determine if the CORI Surgical System is right for you. Children, pregnant women, patients who have mental or neuromuscular disorders that do not allow control of the knee joint, and morbidly obese patients should not undergo a CORI-enabled procedure. The information listed in this brochure is for informational purposes and is not meant as medical advice. For more information, please talk to your surgeon.
◊Trademark of Smith+Nephew.
© 2020 Smith+Nephew
References
* Partial knee replacement vs conventional techniques
- Sephton BM, Bakhshayesh P, Edwards TC, Ali A, Kumar Singh V, Nathwani D. Predictors of extended length of stay after unicompartmental knee arthroplasty. J Clin Orthop Trauma. 2019. 11(Suppl 2):S239-45
- Canetti R, Batailler C, Bankhead C, Neyret P, Servien E, Lustig S. Faster return to sport after robotic-assisted lateral unicompartmental knee arthroplasty: a comparative study. Arch Orthop Trauma Surg. 2018;138(12):1765-1771
† n=28 (n=11 robotic procedures) - Al-Shaer DS, Ayoub O, Ahamed NA, Al-Hibshi AM, Baeesa SS. Cerebral fat embolism syndrome following total knee replacement causing a devastating neurocognitive sequelae 2016 Jul; 21(3): 271-274
- Battenberg AK, Netravali NA, Lonner JH. A novel handheld robotic-assisted system for unicompartmental knee arthroplasty: surgical technique and early survivorship.J Robot Surg.
- Batailler C, White N, Ranaldi FP, et al. Improved implant position and lower revision rate with robotic assisted unicompartmental knee arthroplasty.Knee Surg Sports Traumatol Arthrosc.2019;27:1232.
- Herry Y BC, Lording T, Servien E, Neyret P, Lustig S. Improved joint-line restitution in unicompartmental knee arthroplasty using a robotic-assisted surgical technique.Int Orthop.2017;41:2265-2271.
- Gregori A, Smith JR, Picard F, Lonner JH, Jaramaz B. Accuracy of imageless robotically assisted unicondylar knee arthroplasty. Paper presented at: International Society for Computer Assisted Orthopaedic Surgery (CAOS) 15th Annual Meeting; 2015; Vancover, Canada.
- Bollars P, Boeckxstaens A, Mievis J, Kalaai S, Schotanus MGM, Janssen D. Preliminary experience with an image?free handheld robot for total knee arthroplasty: 77 cases compared with a matched control group. Eur. J. Orthop Surg Traumatol. 2020;30(4):723-9
- Sharkey PF, Hozack WJ, Rothman RH, Shastri S, Jacoby SM. Why Are Total knee Arthroplasties Failing Today?Clinical Orthopaedics and Related Research.2002;404:7-13
- Bollars P, Boeckxstaens A, Mievis J, Janssen D. The Learning Curve and Alignment Assessment of an Image-Free Handheld Robot in TKA: The First Patient Series in Europe. Poster presented at: 19th Annual Meeting of the International Society for Computer Assisted Orthopaedic Surgery. 2019; New York, USA.
- Kopjar B, Schwarzkopf R, Chow J, et al. NAVIO Robotic Assisted Surgical System for Total Knee Arthroplasty Using JOURNEY II Guided-Motion Total Knee System. Poster presented at: ISTA 2-5 October, 2019; Toronto, Canada.
- 00225 V3 JOURNEY II Design Rationale 11.17.
- Shearman AD, et al. Robotic-assisted unicondylar knee arthroplasty is associated with earlier discharge from physiotherapy and reduced length of stay compared to conventional navigated techniques. EKS Arthroplasty Conference. May 2-3, 2019; Valencia, Spain
‡ n=62 (31 robotics) - Smith+Nephew 2020. Comparison of the number of available implants for robotic-assisted knee arthroplasty systems. Internal Report. EO.REC.PCS015.001.v1
- Heyse TJ, Chen DX, Kelly N, et al. Matched-pair total knee arthroplasty retrieval analysis:Oxidized zirconium vs. CoCrMo. The Knee. 2011;18:448-452.
- Papannagari R, Hines G, Sprague J and Morrison M. Long-term wear performance of an advanced bearing knee technology. ISTA, Dubai, UAE, Oct 6-9, 2010
- https://www.arthritis.org/diseases/osteoarthritis. Accessed 22 Oct 2020
- Gregori A, Picard F, Bellemans J, Smith JR, Simone A. Handheld Precision Sculpting Tool for Unicondylar Knee Arthroplasty. A Clinical Review. Poster presented at: 15th EFORT Congress;4-6 June, 2014; London, UK
- Geller JA, Rossington A, Mitra R, Jaramaz B, Khare R, Netravali NA. Rate of learning curve and alignment accuracy of an image-free handheld robot for total Knee Arthroplasty. European Knee Society Arthroplasty Conference;2019; Valencia, Spain.
- Mitra R, Jaramaz B, Nikou C, Kung C. Accuracy Assessment of a Novel Image-Free Handheld Robot for Knee Arthroplasty in Bi-Cruciate retaining knee and total knee replacement – A Cadaveric Study. World Arthroplasty Congress;2018; Rome, Italy.
- Kaper BP, Villa A. Accuracy and Precision of a Handheld Robotic-guided Distal Femoral Osteotomy in Robotic-assisted Total Knee Arthroplasty. European Knee Society Arthroplasty Conference;2019; Valencia, Spain
Our knees are central to maintaining our mobility and allowing us to enjoy our favorite activities. Our quality of life can be impacted when our knees fail due to injury, disease, or a degenerative condition. Dr. Jaime Hernandez is dedicated to providing high-quality replacement options to patients throughout southern California. We achieve exceptional results using the latest innovations in knee-replacement surgery and a commitment to personalized care.
Discover Knee Replacement Treatments With Dr. Hernandez
When experiencing joint pain, we can find that our options and freedom are deeply impacted by how it limits our movement. Our knees are critical to our mobility and are subjected to significant pressures as we move throughout the day. Joggers and runners experience even greater pressure on their knees as they engage in these activities.
Our knees are made of 5 primary components:
- Bones – Three bones form the structure of the knee, the femur, tibia, and patella. The patella, or knee cap, sits in front of the joint to protect it from impact.
- Cartilage – Protecting the ends of the bones making up the knee joint is a layer of cartilage. This material is smooth and durable, limiting friction and providing cushioning that allows the joint to move smoothly.
- Ligament – Strong bands of connective tissue connects bones. Four ligaments exist within the knee structure, the anterior cruciate ligament (ACL), the posterior cruciate ligament (PCL), the medial collateral ligament (MCL), and the lateral collateral ligament (LCL).
- Menisci – Two wedge-shaped pieces of cartilage, individually referred to as the meniscus, are found between the femur and tibia. They function to distribute the forces evenly while boosting stability. They are the shock absorbers of the joint.
- Synovium – The entirety of the joint is enclosed with a thin, delicate lining known as the synovium. This lining creates the synovial fluid that lubricates and nourishes the cartilage.
Knee replacement helps to address various concerns impacting the function of your knee joint. The process’s specific steps depend on your knee’s specific needs. However, the following steps are common:
- Preop Consultation – During this stage, the health of your joint will be assessed, and the surgery details will be decided upon. This stage often involves receiving various forms of imaging,
- Anesthesia – Before receiving surgery, anesthesia will be delivered. With minimally-invasive surgery, you’ll only need a regional anesthetic to numb the area for treatment. General anesthesia will be used in the case of traditional surgery.
- Bone Modification – The bones will have all damaged portions removed and the surfaces prepared to take the artificial implant.
- Implant Placement – The implant will be placed once the area is prepared. The implant is made of high-density plastic and metal alloys. Depending on the nature of your replacement, you may include a plastic spacer, a metal tibial component, and a metal femoral component.
- Patellar Resurfacing (Optional) – The undersurface of the kneecap may also be smoothed and resurfaced with a plastic component.
- Joint Stability and Alignment – The alignment and stability of the joint will be checked to ensure success.
Experience Exceptional Care With Dr. Jaime Hernandez
Following your procedure, the most crucial thing is keeping up with your recovery process. Dr. Hernandez will provide you with an outline to ensure you heal correctly. If you’re ready to experience relief from your knee pain and restore your quality of life, call us today at 805-497-7015 to get your knee replacement in southern California.